RENAL IMAGING
Renal imaging is a reliable method of
evaluating the structure, location and function of the kidneys. The kidneys
regulate the volume and composition of the body’s extracellular fluid through
their excretory function. The kidneys are retroperitoneal organs located
between 12th thoracic and 4th lumbar vertebrae. The right
kidney is positioned slightly lower than the left due to the presence of the
liver superiorly. The kidneys receive blood from the right and left renal arteries,
which branch directly off the descending aorta.
There are three processes
involved in urine formation
1. Glomerular
filtration – involves the filtration of water and solutes out of the glomeruli
and into Bowman’s capsule.
2. Tubular
reabsorption – occurs in the walls of renal tubules and collecting systems,
where most of the water and other physiologically important substances are
reabsorbed into the blood.
3. Tubular
secretion – also occurs in the tubular cells and involves the secretion of
certain substances out of the blood and into the filtrate.
Clinical indications of renal
imaging
1. Evaluation
of renal perfusion and function
2. Evaluation
of renal trauma
3. Diagnosis
of renovascular hypertension
4. Detection
and evaluation of renal collecting system obstruction
5. Evaluation
of renal transplant
6. Diagnosis
of acute and chronic pyelonephritis
7. Differentiation
of renal masses from normal variants
8. Quantification
of regional renal function
A. GLOMERULAR
FILTRATION RATE (GFR)
GFR – is
defined as the volume of plasma filtrate produced in 1 minute by renal
glomeruli of both kidneys. The normal value is 125 ml/minute.
Click
here for Kidney Function Test
Radiopharmaceutical
used:
1. Tc99m–DTPA
(diethylenetriaminepentaacetic acid)
2. Tc99m
– Gluceptate
3. Dose:
3 – 10 mCi
Energy window : 20% window centered at 140 keV
Matrix size : 128 x 128
Patient
preparation:
1. The
patient should hydrate by drinking at least one large glass of water 30 minutes
prior to the study. One suggested protocol is 7 ml of water/kg body weight.
2. The
patient should void before beginning the study.
3. Get
the patient’s age, height and weight as it is included in the quantitation
Interventional
procedure:
1.
Transplanted
kidney
a. The
patient is positioned supine.
b. Images
are acquired in the anterior projection.
c. The
field of view includes the transplanted kidney and bladder (usually imaging the
entire pelvis will accomplish this).
2.
Diuretic
renography
a. The
purpose of this is to rule out any urinary tract obstruction. Furosemide is
administered intravenously to increase urine production. Increased urine flow
will promptly washout the residual tracer activity if there is no obstruction.
3.
Angiotensin
converting enzyme (ACE) inhibitor renal study – for renal artery stenosis
a. Enaprilat:
0.04 mg/kg (40 µg/kg) but not
exceeding 2.5 mg but not
exceeding 2.5
mg infused over 5 minutes.
Note: Enaprilat has a higher
incidence of hypotension so an
intravenous line
with normal saline is suggested
b. Captopril: 25 – 50 mg orally, preferably
crushed in 150 – 250 ml water
Note: Since food in the
gastrointestinal tract delays absorption, the
patient should
fast for 4 hours prior to the study if captopril
will be used.
Click
here for Pharmacokinetics of drugs
c. Blood
pressure should be monitored every 15 minutes for 1 hour
d. A
baseline quantitative renal study should be acquired before captopril study or
2 days after captopril study.
Normal
findings
Normal kidneys
demonstrate prompt tracer uptake with peak uptake at 3–5 minutes. The kidney
activity then gradually decreases as the tracer is excreted. Renal pelvis and
bladder activity is usually seen by 3–6 minutes. The computer generated curves
represent three phases:
1.
Vascular phase – reflects
the arrival of the bolus of activity at the renal area.
2.
Secretory
phase
– tracer is extracted from the renal tubules and to a smaller extent, filtered
by the glomerulus. The peak transit time, usually 3 – 5 minutes following
injection, is the time at which the tracer reaches its maximum concentration in
the kidneys.
3.
Excretory
phase
– follows with a fairly rapid drop in the activity curve as the tracer is
excreted from the kidney into the bladder.
Abnormal
findings
1. Abnormalities
of the renogram curve are usually reflected in the 2nd and 3rd
phase of the renogram curve. An activity curve that exhibits an adequate
upslope but no subsequent fall in activity is usually due to obstruction and
indicates that the renal tubules take up the material but cannot excrete the
activity.
2. A
curve that displays a below normal level of activity throughout the curve
denotes poor renal function. Serial images corresponding to the curve provide
additional visual demonstration of the abnormalities.
Renovascular
hypertension
is estimated to affect 1 – 3% of unselected hypertension population and up to
15 – 30% of patient’s referral to a subspecialty center because of refractory
hypertension.
Renal artery
stenosis
is common in non–hypertensive elderly persons and is an associated but non–etiologic
finding in a number of hypertensive patients.
Renovascular
hypertension
is defined as an elevated blood pressure caused by renal hypoperfusion, usually
due to anatomic stenosis of the renal artery and activation of the renin–angiotensin
system. The goal of a screening test is to detect those patients who have renal
artery stenosis as the cause of hypertension and hopefully to predict
curability of hypertension following hypertension.
Clinical
features associated with moderate to high risk renovascular hypertension
includes:
1. Abrupt
or severe hypertension
2. Hypertension
resistant to medical therapy
3. Abdominal
or flank bruits
4. Unexplained
azotemia
5. Worsening
renal function during therapy with ACE inhibitors
6. Grade
3 or 4 hypertensive retinopathy
7. Occlusive
disease in other vascular beds
8. Onset
of hypertension under age 30 or over age 55
Image
acquisition
1. When
the 2 days protocol is performed, ACEI renography should be done on the first
day. If the ACEI renogram is normal, the chance that the patient has
renovascular hypertension is low and there is no need to have the patient
return on the second day for a baseline study.
2. When
the one day protocol is performed, baseline renography should be
performed first with only 1 mCi of Tc99m DTPA or MAG3. The
administered activity for the ACEI renogram should be 5 – 10 mCi in order to
overwhelm any counts from the baseline study.
Precautionary
measures
1. Tc99m
MAG3 is preferred over DTPA in patients with elevated creatinine
because of its higher extraction
2. Since
the furosemide is a loop diuretic, it can wash the radiopharmaceutical out of
the calyces and pelvis and improve evaluation of cortical retention of tubular
agents MAG3 and OIH. It can also cause volume depletion and increase
the risk of hypotension.
3. The
renal uptake of MAG3 and OIH, should be measured in each kidney in
the 1 – 2.5 minutes (3 minutes for DTPA) interval. Since after 2.5 minutes, a
portion of the tracer have already left renal parenchyma and accumulated in the
collecting system thus leading to incorrect estimates. Exclusion of the pelvis
and calyces is important if there is retention of activity in these structures.
Interpretation
of results
ACEI
renography has a sensitivity and specificity of about 90% for diagnosis of
renal artery stenosis. Most importantly, ACEI–induced renographic findings of
renovascular hypertension indicate a high probability that blood pressure will
reduce after intervention.
1. Low
probability
Abnormal
baseline findings that improve after ACE inhibition
2. Intermediate
probability
Abnormal
baseline findings but the renogram is unchanged after ACE inhibition. This
group includes some azotemic patients and hypertensive patients who have a
small, poorly functioning kidney.
3. High
probability
a. For
MAG3 and OIH – a change in 20 min/peak ratio of 0.15 or greater or a
significantly prolonged transit time or by a change in the renogram grade. It
can also be detected as a delay in the excretion of the tracer into the renal
pelvis >2 minutes following ACEI or an increase in the Tmax of at
least 2 minutes or 40%.
b. For
DTPA – reduction in relative uptake greater than 10% after ACEI or 10% decrease
in calculated GFR of the ipsilateral kidney after ACEI or marked unilateral
parenchymal retention after ACEI compared to baseline study.
Renographic
curve pattern
0
– Normal
1
– Minor abnormalities
2
– Marked delay excretion rate with present washout phase
3
– Delayed excretion without washout phase
4
– Renal failure pattern with measurable kidney uptake
5
– Renal failure pattern without measurable kidney uptake (blood background
Type
curve)
B. TUBULAR
FUNCTION
Effective
renal plasma flow (ERPF) – is a measurement of renal tubular
function. The “term” effective is used to describe the measurement of renal
plasma flow.
Radiopharmaceutical
used:
1. Tc99m–DMSA
(dimercaptosuccinic acid)
2. Orthoiodohippurate
(I131 OIH)
Energy window: 20% window centered at 140 keV
Procedure of
the test:
1. An
injection of 5 mCi Tc99m–DMSA is instituted.
2. After
3 hours, patient is positioned supine.
3. Acquire
the following view: anterior, posterior, right anterior oblique, left anterior
oblique, right posterior oblique, left posterior oblique at 400k.
4. Acquire
SPECT images with the following parameters:
Degree of
rotation : 360o
Number of images : 64
Time per image : 20 seconds
Normal
findings
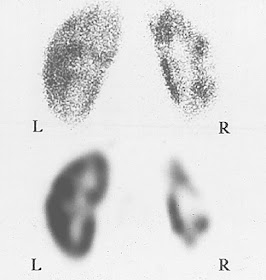
Normal static
images obtained 1 hour or more after injection demonstrates a smooth renal
contour. Tracer distribution within each kidney should be uniform and both
kidneys should have equal tracer concentration.
Abnormal
findings
Congenital
malformations such as fetal lobulations and horshoe kidneys are easily
identified on the images as areas of activity outside the normal renal outline.
Areas of increased or decreased radioactivity may represent cyst, neoplasms,
infarcts or renal trauma.
Technical
considerations
If the patient
is in severe renal failure, images obtained with DMSA may need to be delayed up
to 24 hours to improve visualization of the kidneys. Horshoe kidneys and pelvic
kidneys are located more anteriorly than the normal renal position. If these
anomalies are a consideration, an anterior projection may be helpful.
C. TUBULAR
SECRETION
MAG3
is handled solely by tubular secretion and has an overall clearance that is
less than that of OIH. It has the better physical characteristics of Tc99m.
Millicurie amounts of MAG3 can be administered to patients, thus
resulting in higher counting statistics and better image resolution.
The renal
tubular secretion images Tc99m–MAG3 as it passes through the
vascular system, renal tubular cells, tubular lumens and collecting systems.
This series of images allows the sequential evaluation of renal perfusion,
renal clearance by tubular secretion, renal parenchymal transit time and is passage
of urine through the renal collecting system. In addition, the study provides
high contrast images for evaluation of renal anatomy.
Radiopharmaceutical
used:
1. Tc99m–mercaptoacetyltriglycerine
(MAG3)
Energy window : 20%
centered at 140 keV
Matrix size : 128 x 128
Procedure of
the test : Same as GFR
Quantitative renal studies:
Quantitative techniques provide
numerical values that indicate the level of tubular and glomerular function. In
addition to the renogram curve and nuclear medicine images such values are
useful in monitoring the course of patients with many different types of renal
pathology. Quantitative studies are based on either a blood sampling technique
to estimate tracer clearance from the blood or a camera method to determine the
amount of tracer accumulated in the kidneys. The advantage of radionuclide
technique over chemical measurements such as creatinine clearance is that the
function of each kidney (differential function) can be determined.
RADIONUCLIDE
CYSTOGRAPHY
Radionuclide cystography is performed
for the evaluation of vesicourethral reflux, which is common in children. This
condition is often responsible for recurrent urinary tract infection, which may
damage the kidney.
This study is more sensitive than radiographic
methods because of high contrast between instilled radioactivity in the bladder
and the lack of radioactivity outside the bladder.
Radiopharmaceutical used
1. Tc99m–sulfur
colloid
2. Tc99m–sodium
pertechnetate
3. Tc99m–DTPA
Two methods of performing
cystography
1.
Indirect
method
– involves intravenous administration of a renal agent. After the agent is
cleared from the kidneys into the bladder, the patient is asked to void while
being imaged. Reflux that occurs during voiding can then be observed.
2.
Direct method – most
commonly used
a. Have
patient void before the study.
b. Catheterize
the patient.
c. Connect
the catheter to a bottle of normal saline to which 1 mCi pertechnate has been
added.
d. Position
the patient supine on the imaging table with the upper portion of the bladder
in the lower part of the field of view.
e. Obtain
multiple sequential images as the bladder is being filled with radionuclide
saline solution.
f.
Discontinue saline infusion
when bladder capacity is reached. Obtain a posterior pre–void image that
includes the entire bladder and upper urinary tracts.
g. Obtain
voiding images with the patient in the seated position and the camera against
the patient’s back. Remove the catheter and encourage the patient to void into
a bed pan or urinal.
Image findings
The normal exam will demonstrate
increasing activity in the bladder without reflux into the ureters. The
abnormal exam will demonstrate ureteral reflux, especially during micturition.
Reflux usually increases as the study progresses, although transient reflux may
occur.
Certain quantitative information, such
as the reflux bladder volume and volume of reflux into the kidney, can also be
calculated.
Technical considerations
1. Equipment
and the surrounding area should be covered with absorbent paper to prevent
contamination with radioactive urine.
2. It
is important to establish adequate bladder filling before the voiding portion
of the exam. An increase in patient discomfort, leakage of urine around the
catheter or cessation of flow from saline infusion bottle may all indicate
sufficient bladder filling. Bladder capacities vary according to age and
condition of the bladder.
3. If
quantitative results are desired, not that any loss of urine will cause
inaccuracies in the calculation.
4. Children
may not cooperate when asked to void, depending on their age.
5. Catheterization
should be performed by someone who is well trained in the technique to ensure
correct placement and to avoid physical or psychological trauma to the child.
SCROTAL
IMAGING
Scrotal imaging is most often
performed to differentiate acute torsion (twisting) of the spermatic cord and
epididymitis. Torsion of the spermatic cord is often spontaneous and occurs
most commonly in young men, with an acute onset of pain. The distinction is
important since torsion requires immediate surgical intervention while
epididymitis requires antibiotic therapy.
Tc99m pertechnetate is the usual
tracer used. Sequential images of the scrotum are acquired for 5 minutes each
for up to 30 minutes. Lead is also put beneath the scrotum to obscure
background uptake.





No comments:
Post a Comment
Note: Only a member of this blog may post a comment.