EOSINOPHIL COUNT
The procedure for
eosinophil count consists of diluting the blood with an eosinophil diluting
fluid, charging a counting chamber, counting the eosinophils through the
microscope, and making the calculation.
Equipment
1.
White cell pipette
2.
Eosinophil diluting fluid
3.
Cotton balls and alcohol
4.
Sucking tube
5.
Puncturing device
6.
Microscope
7.
Counting chamber which maybe any of the following:
a. Improved Neubauer ruling counting
chamber
b. Fuchs–Rosenthal counting chamber
c. Speirs–Levy counting chamber
Eosinophil diluting
fluid
1. Phloxine diluting fluid
Propylene
glycol – 50 ml
Distilled
water – 40 ml
1%
aqueous solution of phloxine – 10 ml
10%
aqueous solution of sodium carbonate – 1 ml
2. Pilot’s solution
This
has the same composition as phloxine diluting fluid except that 100 units of
heparin should be added. Heparin keeps the cells clumping. Sodium carbonate
lyses all white cells except eosinophils. Phloxine stains the eosinophils red.
Propylene glycol renders the red cells invisible
3. Dunger’s diluting fluid
2%
aq. Eosin – 5 cc
Acetone
– 5 cc
Distilled
water – 90 cc
4. Manner’s diluting fluid
Urea
– 50 g
Distilled
water – 100 ml
Trisodium
citrate – 0.5 g
Phloxine
– 0.1 g
5. Randolph’s diluting fluid
Phloxine
– 0.1 g
1%
calcium chloride – 100 ml
Propylene
glycol – 100 ml
6.
Tannen’s diluting fluid
Neutral
red iodide solution (0.2%) – 100 ml
0.1 N NaOH – 2.1 ml
7. Hinklemann’s fluid
Eosin
yellow – 0.5 g
Formaldehyde
– 0.5 g
95%
phenol – 0.5 ml
Any of the following
three types of counting chamber may be used
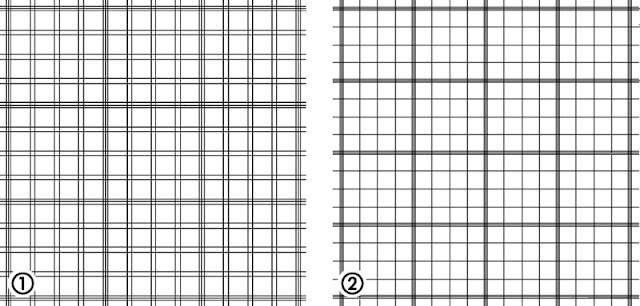
1. Improved Neubauer Ruling Counting Chamber
It
has 2 ruled section; each section has an area of 9 sq.mm and a depth of 0.1mm.
Therefore, the volume of 1 section is 9 x 0.1 = 0.9 cu.mm. and the volume of 2
sections is 2 x 0.9 = 1.8 cu.mm.
2. Fuchs–Rosenthal Counting Chamber
This
counting chamber has 2 ruled sections; each has an area of 16 sq.mm. (has 16
big squares). Each is further subdivided into 16 medium squares. It has a depth
of 0.2mm. Therefore, the volume of 1 section is 16 x 0.2 = 3.2 cu.mm. and the
volume of 2 sections is 2 x 3.2 = 6.4 cu.mm.
3. Speirs–Levy Counting Chamber
This
chamber has 4 sections. Each section has an area of 10 sq.mm. and a depth of
0.2 mm. each sq.mm. is further subdivided into 16 medium squares. Therefore,
the volume of 1 section is 10 x 0.2 = 2 cu.mm. and the volume of the four
section is 4 x 2 = 8 cu.mm.
Methods of eosinophil
count:
1. Randolph’s method
Counting
chamber used – Improved Neubauer
No.
of squares counted – 9 big squares
Area
in sq mm – 9 sq.mm.
Depth
of chamber – 0.1 mm
Volume
where actual count is done – 0.9 cu.mm.
Area
correction factor – 1/9
Depth
correction factor – 10
Volume
correction factor – 1/0.9
Ratio
of dilution – 1: 10
Dilution
correction factor – 10
Computation:
E
in big squares x 10 = E/cu.mm
0.9
E/cu.mm
x 0.001 = x 109/liter
2. Thorn’s method
Counting
chamber used – Fuchs – Rosenthal chamber
No.
of squares counted – 16 big squares
Area
in sq.mm – 16 sq.mm
Depth
of chamber – 0.2 mm
Volume
where actual count is done – 3.2 cu.mm
Area
correction factor – 1/16
Depth
correction factor – 10/2 or 5
Volume
correction factor – 1/3.2
Ratio
of dilution – 1:10
Dilution
factor – 10
Computation
E
in 16 big squares x 10
= E/cu.mm
or ul
3.2
E/cu.mm
x 0.001 =
x 109/liter
3. Speir’s method
Counting
chamber – Speirs – Levy chamber
No
of squares counted – 4 sections of 10 squares ( 40 squares in all)
Area
in sq.mm – 40 sq.mm
Depth
of chamber – 0.2 mm
Volume
where actual count is done – 8 cu.mm
Area
correction factor – 1/40
Depth
correction factor – 5
Volume
correction factor – 1/8
Ratio
of dilution – 1:10
Dilution
factor – 10
Formula
E
in 40 big squares x 10
= E/cu.mm
or ul
3.2
E/cu.mm
x 0.001 =
x 109/liter
4. Friedman’s method
Technique
and method of calculation are the same as Randolph’s method. It uses a diluting
fluid which stains the eosinophils only and the unstained leukocytes stay as
gray bodies.
5. Pilot’s method
Counting
chamber – Improved Neubauer
No.
of squares used – 4 sections of 9 squares each
Area
in sq.mm. – 16 big squares
Area
correction factor – 1/16
Depth
factor – 1:10
Volume
factor – 3.6
E
in 36 big squares x 10
= E/cu.mm
or ul
3.2
E/cu.mm
x 0.001 =
x 109/liter
Formula to obtain the %
value of eosinophils
Eosinophils / cu.mm. x 100 = %
of eosinophils
Total WBC / cu.mm
Normal value: 0 – 4.5 x 109/liter
Thorn’s ACTH Test
This test is based on the
fact that Adrenocorticoptropic Hormone (ACTH) produces in 4 hours a decrease by
50% or more in the eosinophil count of persons with a normally functioning
adrenal cortex. It is useful as a diagnostic test in Addison’s disease, as a
test for adrenal cortex reserve before surgical procedures, and a test to
distinguish functional form organic disease of the adrenal cortex.
ABSOLUTE BASOPHIL COUNT
Toluidine Blue Method
(Cooper’s method)
Cetylpiridium chloride is
used to lyse the erythrocytes and to render the basophil granules insoluble.
Aluminum sulfate is used as a mordant to improve the staining qualities of
toluidine blue. EDTA prevents platelet agglutination.
Staining solution:
0.1% EDTA in saline solution – Solution I
Cetylpiridium chloride (0.5%) – 25 ml
Distilled water – 25 ml
Toluidine blue (0.8%) in aluminum sulfate – 20 ml
Procedure:
0.08 ml of Solution I and
0.02 ml finger blood is mixed. Add 0.1 ml Solution II. Mix and stopper. Charge
2 Fuchs – Rosenthal chambers using a Pasteur pipette. Allow 5 minutes for the
cells to settle.
Computation:
B
in 16 big squares x 5
= B/cu.mm
or ul
16
Depth
of the chamber – 0.2
Depth
factor – 5
Volume
in cu.mm – 3.2 (one section); 6.4 (2 sections)
No
dilution employed so no dilution factor
Neutral Red Method
This is another
staining method for basophils. But is has the following disadvantage:
1.
Eosinophils may also stain
2.
Basophil granules may be water soluble
3.
Platelet aggregates may interfere with the count
Indication of basophil
count
1. Allergic conditions
2. Sensitization and anaphylaxis
Sensitization
leads to an increase in the number of basophils which level too when the
sensitization has occurred. If the patient is challenged with the same antigen,
the count will fall at the rate depending on the type of reaction. Anaphylaxis
leads to a rapid fall.
Normal
values: 0 – 0.2 x 109/liter
RETICULOCYTE COUNT
Reticulocytes are juvenile
red cells; they contain remnants of the ribosomes and the ribonucleic acids
which were present in larger amounts in the cytoplasm of the nucleated
precursors from which they were derived. They possess a network known as
reticular filamentous substance or granulo–filamentous substance which can be
recognized on supravital staining. This characteristic is utilized for counting
reticulocytes. The reticulum may be abundant or sparse depending on the
maturation of the erythrocytes.
The number of
reticulocytes in the peripheral blood is fairly accurate reflection of
erythropoeitic activity, assuming that there is normal release of reticulocytes
from the bone marrow, and that remain in circulation for the normal period of
time.
The reticulocyte count can
be made either with the use of dry or wet method.
Dry method:
The dry method consists of
mixing blood and a special staining solution to stain the reticulocytes, using
the mixture to make the smear, counterstaiing the smear with Wright’s stain,
counting 1,000 red cells with the microscope, and calculating the % of
reticulocytes.
Wet method:
The wet method consists of
spreading a film of stain on a glass slide, adding a drop of blood, covering
the preparation with a coverglass, counting 1,000 red cells with the microscope
and calculating the % of reticulocytes.
Methods of reticulocyte
count
1. New methylene blue
New
Methylene Blue N method
New
Methylene Blue N – 0.5 g
Potassium
oxalate – 1.4 g
Sodium
chloride – 0.8 g
Distilled
water – 100 ml
2. Cook, Meyer and Tureen method
Solution
A: 1% saline solution of Brilliant
Cresyl Blue
Solution
B: 1% saline solution of Potassium
oxalate
3. Seiverd’s method
a.
1% physiologic saline solution of Brilliant Cresyl Blue
b.
1% methyl alcohol solution of Brillian Cresyl Blue
c.
New methylene blue N solution
4. Rapid method of Schilling
1%
alcohol solution of Brilliant Cresyl Blue
5. Sabin’s method
a. Neutral red solution
Neutral
red special – 125 mg
Neutral
absolute ethyl alcohol – 50 ml
b. Janus Green solution
Janus
green special – 125 mg
Neutral
absolute alcohol – 62.5 ml
6. Osgood–Welhelm method
New
Methylene Blue N method
Computation
Number of retics counted x 100 = %
Retics
1000 red cells (retics & RBC)
% Retics x RBC count/cu.mm = retics/cu.mm
100
Retics/cu.mm x 0.001 = x
109/liter
Corrected Reticulocyte count:
% Retics x Patient hematocrit = Corrected
reticulocyte in %
Norma hematocrit
The normal hematocrit reading is taken to be 45%
Normal values
0.5 – 1.5% or
5 – 15 x 10–3 / liter
25,000 – 75,000 or 25
– 75 x 109/ liter
Importance
of Reticulocyte count
1. To determine the response of the pernicious anemia patient to Vitamin
B12 therapy
2. To aid in the diagnosis of hemolytic anemia and lead poisoning
3. To determine whether regeneration of erythrocytes is processing
normally and whether it occurs at all that is of value in establishing a
diagnosis of aplastic anemia.
4. To aid in the diagnosis of acute hemorrhage.
Reticulocyte
is increased in: (Reticulocytosis)
1.
Hemolytic anemias
2.
Lead poisoning
3.
Malaria
4.
Parasitic infestations
5.
Toxic granulation
It
is increased in
1. Aplastic anemia
2. Acute benzol poisoning
3. Chronic infections
SIDEROCYTE COUNT
Siderocytes are
erythrocytes containing granules which give a positive Prussian blue or Perls
reaction for iron. The iron containing granules of siderocyte appear as
basophilic granules. These granules are called Pappenheimer bodies when blood
smears are obtained with Romanowsky stain (Wright’s solution) wherein they
appear as basophilic rods or grains.
When the smears are first
stained for reticulocytes with New Methylene Blue N and then stained with
Safranin O, reticulum stains red and siderotic granules stain blue. Therefore,
cell may be differentiated into those that:
a. Contain siderotic granules with no reticulum (siderocytes)
b. Those containing reticulum with no siderocytic granules (reticulocytes)
c. Those that contain both reticulum and siderotic granules (reticulated
reticulocytes)
Prussian
Blue or Perl’s reaction
Douglas
or Dacie’s method
Prussian blue reagent
20% potassium ferrocyanide solution
Concentrated HCl
Safranin O counterstain
Safranin O – 0.5 grams
Distilled water – 100 ml
Computation:
No.
of siderocytes and reticulated siderocytes x 100 = % siderocytes
1000
red cells (includes siderocytes & reticulocytes
No.
of retics and reticulated siderocytes
1000
red cells (includes siderocytes and retics x 100 = % reticulocytes
No.
of siderocytes only (if only one stain was used) x 100 = % siderocytes
1000
red cells (including siderocytes)
The
siderocyte stain is useful in differentiating anemia due to iron deficiency
from anemia or thalassemia or other disorders in which iron accumulates because
it is poorly utilized for hemoglobin synthesis.
PLATELET COUNT
Blood
collection for platelet count
1. For best results, collect the blood with a 20 gauge needle and a
siliconized syringe. Transfer the specimen to a small siliconized test tube
which is kept cool either in an ice bath or in a refrigerator.
2. Capillary blood from a finger puncture may be diluted directly in a
leukocyte or erythrocyte pipette.
3. Collect the blood in a non–siliconized syringe and transfer to a test
tube containing EDTA.
Platelets are thin disks,
2 to 5 micrometers in diameter and 5 to 7 femtoliters in volume. They are
small, colorless, moderately refractile bodies. When stained, they appear as
azure granules with scanty blue cytoplasm.
Platelets are difficult
to count because:
1. They are small and hard to distinguish from debris
2. They easily disintegrate
3. They have the tendency to adhere to glass, to any foreign body and
particularly to each other
Methods of platelet
count
1. Indirect method
In
this method, platelets are counted in their relationship to red cells on a
fixed smear. This is not reliable because the result depends upon the
distribution of platelets and on the red blood cell count.
a. Fonio’s method
Stain
used: 14% Magnesium sulfate
Wright’s stain
b. Dameshek’s method
Stain
used: Brilliant
Cresyl Blue
Wright’s stain
c. Olef’s method
Formula
No.
of platelets counted on the smear x RBC count/mm3
1000
(red cells counted on the smear)
=
Platelet / cu.mm.
2. Direct method
In
this method, the platelets are counted in the counting chamber as in leukocyte
or erythrocyte count
a. Reese and Ecker’s method
Diluting
fluid: Sodium citrate – 3.8 g
Formalin – 0.9 ml
Brilliant Cresyl
Blue – 0.1 g
Distilled water
q.s.ad – 100 ml
b. Leake and Guy’s method
Diluting
fluid: Sodium oxalate – 1.6 g
40% Formalin – 94
ml
Crystal violet –
0.05 g
Computations:
If
blood is diluted 1:20 with WBC pipette and 5 medium squares are counted, the
formula is:
No. of P seen in 5 squares x 5 x 10 x 20
= P/cu.mm
If
blood is diluted 1:200 with the RBC pipette and 4 big squares (WBC squares) are
used, the formula is:
No.
of P seen in 4 big squares x 10 x 200 = P/cu.mm
4
P/cu.mm
x 0.001 = 109/liter
c. Brecker–Cronkite method
In
this method, the platelets are identified on the basis of their size, shape and
structure with the use of phase – contrast microscope. The platelets under this
type of microscope can easily be identified and readily distinguished from
debris, precipitated stain and other foreign materials.
Diluting
fluid: 1% ammonium oxalate
Ratio
of dilution: 1:100
No.
of P in 5 squares x 5 x
10 x 100
= P/cu.mm x
0.001 = x 109/liter
d. Electronic method of platelet counting
(1)
Voltage–pulse counting
Dilution: 1:3000
3 ul blood plus 9 ml
isoton or NSS
For
platelelt count of less than 250,000/ul, the dilution is 1:300 – 20 ul plasma
plus 6 ml diluent.
(2)
Electro–optical counting
Dilution:
1:1500 – in 2M area
Normal
values
Indirect method 250 – 500 x 109/liter
Direct method 150 – 450 x 109/liter
Sources
of error
1. Error in sampling
2. Operator’s error
3. Error in equipment and reagent
4. Inherent error or field error
Physiologic
variation
1. Platelet count is slightly lower
at birth than in older children and adults
2. Platelet count may fall at the
time of menstruation.




No comments:
Post a Comment