General characteristics
1. They are unicellular organisms.
2. They are slender, helically coiled, flexible organisms, motile, resulting from the action of axial filaments which are also responsible for their spiral shape.
3. They
are facultative anaerobes and multiply by transverse fission.
TREPONEMA
Characteristics
1. The word Treponema is derived from a Greek word meaning “turning thread.” They are corkscrew like organisms.
2. The spirals are so thin that they are not readily seen unless darkfield illumination or immunofluorescent stain is employed. They are not stained very well with aniline dyes, but they do reduce silver nitrate to metallic silver that is deposited on the surface so the treponemes can be seen in tissues (Levaditi Silver Impregnation).
3. Pathogenic strains have never been cultured with certainty on artificial media, in fertile eggs, or in tissue culture but maintained in the testicular chancres of rabbits. Non–pathogenic strains (Reiter strain) can be cultured anaerobically in vitro and grow on a defined medium of amino acids, vitamins, salts, minerals, and serum albumin.
4. They remain viable in whole blood or plasma for at least 24 hours which is of potential importance in blood infusion.
5. They are killed rapidly at 42oC and is used as a basis for syphilis therapy.
6. A life cycle has been postulated from Treponema pallidium consisting of granular stage, cyst–like spherical bodies and spirochetal form.
7. There are two types of antibodies produced: reagin, an antibody like substance and antitreponemal antibody, a true antibody, both of which can be used for the serologic diagnosis of syphilis.
TREPONEMA PALLIDUM
Characteristics:
1. It is a microaerophilic gram–negative bacterium that depends primarily on glycolysis for energy production. It is highly sensitive to oxygen and temperature and is not readily maintained in culture.
2. It can be propagated by intratesticular inoculation of rabbits, where it displays a slow replicative cycle of approximately 30 hours.
3. A striking feature of Treponema pallidum and other spirochetes is their capacity to swim efficiently in a highly viscous, gel-like environment, such as connective tissue, where most externally flagellated bacteria are slowed down or stopped.
4. It’s flexuous, flat–wave morphology enables it to penetrate tissues and vascular barriers throughout the body, while its periplasmic motility apparatus propels it forward via front–to–back undulations coordinated in response to poorly understood chemotactic signals.
5. To establish infection, Treponema pallidum must adhere to epithelial cells and the extracellular matrix components; in vitro binding studies suggest that fibronectin and laminin are key substrates for this interaction.
6. They lack lipopolysaccharide (LPS).
Subspecies of Treponema pallidum:
1. TPE (Treponema pallidum subspecies pertenue) – causative agent of yaws or frambesia. It is a tropical skin infection that spreads via direct skin-to-skin contact with an infected lesion and is most prevalent in children between the ages of 2 and 15 years old. It undergoes three stages: primary, secondary, and tertiary. They are separated by a period of latency.
a. Primary stage usually appears 3 – 5 weeks at the site of inoculation like feet, legs, or buttocks. It is a papulonodular lesion of 1 – 5 cm diameter, indurated and painless that grows and ulcerates. The surface is reddish (fambresia) and is covered with a yellowish crust. It heals spontaneously in several weeks or months leaving a hypopigmented area surrounded by a dark halo. There can be fever, joint and regional adenopathy.
b. Secondary stage – appears weeks or months after the primary stage. It is accompanied by headache, fever, malaise, and joint pain, with disseminated lesion smaller than the initial lesion. There are macules, papules, or plaques (daughter yaws or "pianids") that ulcerate and are eczematous. They are seen on joints or around the nose and mouth. Sometimes they are annular or circinate, appearing as macerated condylomas in axilla and groin. There is painful palmar and plantar hyperkeratosis (rough yaws) and periungual papillomas causing paronychia. The secondary lesions are recurrent in the axilla and perianal region, and they can enter in a period of latency.
c. Late stage – appears from 5 – 15 years after the primary infection and it develops in 10 – 15% of patients. There are nodules that darken and ulcerate, palmar and plantar hyperkeratosis and hypertrophic lesions with bone and joint abnormalities. Chronic osteitis causes so called "sabre tibia." Neurologic and ophthalmologic involvement is controversial. Yaws in this stage spares skin folds.
Crab yaws – infection of the feet which causes a crippling form of disease.
Treponema Fribourg–Blanc was isolated in 1966 from Baboons (Papio cynocephalus) in West Africa. The Fribourg–Blanc genome showed similar genetic characteristics as other TPE strains.
2. TEN (Treponema pallidum subspecies endemicum) – causative agent of Bejel, also known as endemic syphilis, it is characterized by lesions of the skin and bones that begin in the mouth and progress in gradual stages.
3. TPA
(Treponema pallidum subspecies pallidum) – causative
agent of syphilis
Adhesion proteins of Treponema pallidum:
1. TP0751 – is a zinc–dependent metalloprotease (hence, was named “pallilysin”) that forms a complex with TP0750 (which contains a Von Willebrand factor type A domain) capable of degrading clots and extracellular matrix, which could facilitate both dissemination and attachment. Pallilysin also degrades laminin, a major constituent of the basement membrane that lines the vascular endothelium and a barrier that Treponema pallidum must pass through during dissemination via the bloodstream.
2. TP0155 and TP0483 – binds fibronectin. Tp0155 preferentially bound the matrix form of fibronectin, whereas Tp0483 bound both the soluble and matrix forms of fibronectin. The two forms of fibronectin exist in different conformational states, with cryptic epitopes becoming exposed during fibronectin matrix assembly.
Antigens of Treponema pallidum:
1. TP0136 – is a fibronectin–binding adhesin with sequence heterogeneity among Treponema pallidum strains. The TP0136 protein is exposed on the surface of the bacterial outer membrane and bound to the host extracellular matrix glycoproteins fibronectin and laminin. It is reactive with sera collected from patients with primary–stage syphilis.
2. TP0435/Tpp17 – has been known for years as a major treponemal antigen with great utility for serodiagnosis of syphilis where it also functions as cytadhesin.
3. Tp1038 – the oligomeric form of this antigen exhibited high antibody responses with all stages of syphilis but did not exhibit serologic reactivity against the monomeric form. Currently this antigen has shown a high sensitivity (93.3 – 100%) for the detection of all stages of syphilis and was extremely specific (100%) when tested against potentially cross–reactive sera, and that proposes Tp1038 to be a promising candidate for the screening of syphilis.
4. TpF1 – an oligomeric protein, belonging to the bacterio–miniferritin family and called as 4D Ag, has been described as a periplasmic antigen, but considering that it induces an important seroconversion, particularly in primary syphilis patients, it is conceivable that a proportion of TpF1 is somehow released by the bacterium.
5. TprK – is an outer membrane β–barrel with porin function and with several surface–exposed loops, seven of which correspond to the variable regions. No definitive structural of functional data, however, exists for this protein aside from its role in immune evasion. TprK is a key virulence factor of Treponema pallidum subspecies pallidum due to its ability to undergo intra-strain antigenic variation through gene conversion.
Serodiagnostic Test category for Syphilis:
1. Nontreponemal Tests (NTTs) – measure immunoglobulins (IgM and IgG) produced in response to lipoidal material released from the bacterium and/or dying host cells. NTTs are useful in detecting active syphilis. However, because individuals with an infection do not become positive until 10 – 15 days after the onset of the primary lesion, 25 – 30% of primary syphilis cases may be missed. These are flocculation (precipitation) tests that detect “nontreponemal antibodies” (also called “reagin”) to a suspension of lecithin (including phosphatidylcholine and phosphatidylethanolamine), cholesterol and cardiolipin.
d. Rapid
Plasma Reagin (RPR)
e. Toluidine
Red Unheated Serum Test (TRUST)
f. Venereal Disease Research Laboratory (VDRL)
2. Treponemal Tests (TTs) – detect antibodies directed against Treponema pallidum proteins and are theoretically highly specific. However, as most individuals infected with syphilis develop treponemal antibodies that persist throughout life, TTs cannot be used to distinguish an active from a past or previously treated infection and are not useful in evaluating treatment effectiveness. TTs are used as confirmatory assays following a positive NTT result.
a. Fluorescent
Treponemal Antibody Absorbed (FTA–ABS) Test
b. Microhaemagglutination
Assay for Antibodies to Treponema pallidum (MHA–TP)
c. Treponema
pallidum passive particle agglutination (TPPA)
d. Treponema pallidum hemagglutination (TPHA) assays
Structure of Treponema pallidum:
1. Outer membrane – consists principally of phosphatidylcholine, phosphatidylglycerol, phosphatidylserine, and an uncharacterized poorly immunogenic glycolipid. Notably absent was lipopolysaccharide (LPS), the highly inflammatory glycolipid responsible for creating the OM permeability barrier in Gram–negatives.
2. Periplasmic space with endoflagella – three to six flagella extends from periplasmic space from both ends toward the center of microorganism and determines the helical shape and characteristic corkscrew motility (rotating around longitudinal axis) of Treponema pallidum cells.
Spirochetes possess periplasmic flagella that confer the ability to effectively translocate in highly viscous gel–like media conditions that would normally hinder other bacteria with external flagella. Unlike most external flagellar filaments, which are composed of a single flagellin subunit, the flagellar filament of Treponema pallidum consists of multiple proteins: FlaB1, FlaB2, FlaB3 and FlaA. FlaA forms an external sheath on the Treponema pallidum flagellar filament, whereas FlaB1, FlaB2, and FlaB3 form the central core.
3. Periplasmic Cone – it was observed at the ends of each organism; this unique feature appears to be comprised of lipoproteins arranged in a helical lattice adjacent to the outer membrane.
4. Flagellar motor – anchored in the cytoplasmic membrane at each end of the cell cylinder and are arranged in a row such that the flagellar hooks are pointing toward the middle of the organism. The function of which is still under investigation.
5. Cytoplasmic filaments – a ribbon–like structure, typically composed of 4–8 filaments anchored to the inner surface of the cytoplasmic membrane. The exact role of cytoplasmic filaments, particularly in Treponema pallidum requires further investigation.
Treponema pallidum infection:
Treponematoses is the collective term that describes the infection caused by Treponema species.
1. Syphilis – is a sexually transmitted disease (STD) from the infection of Treponema pallidum bacteria. It has the following stages:
a. Primary – the lesion of primary syphilis occurs at the site of initial inoculation of Treponema pallidum. It is usually single and painless but can be multiple and painful. It tends to begin as a macule that becomes a papule, which then ulcerates. A 2-to-3-week incubation period usually occurs between the inoculation of Treponema pallidum and development of the lesion (the range of incubation period is reported as being 9-90 days). Local, non-tender lymphadenopathy is often associated with this lesion.
b. Secondary – occurs four to eight weeks after primary syphilis, where it becomes a systemic infection with bacteremia. This secondary stage of syphilis is characterized by a generalized and usually symmetrical macular papular rash, which is often widespread and may also involve the scalp, palms, and soles. Occasionally this rash is predominantly papular, and rarely do these papules ulcerate. This can be associated with generalized lymphadenopathy and mucosal ulceration. These ulcers may coalesce on the buccal mucosa, forming “snail track” ulcers, and in the genital regions (where there are opposing membranes) they can cause wart-like lesions called condylomata lata. These features are often accompanied by constitutional symptoms such as fevers and malaise.
c. Latent – About 35% of individuals with late latent syphilis will develop the late manifestations of syphilis (tertiary syphilis). The three main manifestations of late syphilis are neurosyphilis, cardiovascular syphilis, and gummatous syphilis.
2. Neurosyphilis – is an infection that affects the coverings of the brain, the brain itself, or the spinal cord. It can occur in people with syphilis, especially if their condition is left untreated. There are five types of neurosyphilis:
a. Asymptomatic neurosyphilis means that neurosyphilis is present, but the individual reports no symptoms and does not feel sick.
b. Meningeal syphilis can occur between the first few weeks to the first few years of getting syphilis. Individuals with meningeal syphilis can have headaches, stiff neck, nausea, and vomiting. Sometimes there can also be loss of vision or hearing.
c. Meningovascular syphilis causes the same symptoms as meningeal syphilis but affected individuals also have strokes. This form of neurosyphilis can occur within the first few months to several years after infection.
d. General paresis can occur between three to 30 years after getting syphilis. People with general paresis can have personality or mood changes.
e. Tabes dorsalis is characterized by pains in the limbs or abdomen, failure of muscle coordination, and bladder disturbances. Other signs include vision loss, loss of reflexes and loss of sense of vibration, poor gait, and impaired balance. Tabes dorsalis can occur anywhere from five to 50 years after initial syphilis infection.
3. Cardiovascular syphilis is the third stage of syphilis infection and falls in the category of advanced syphilis. About 10% of untreated patients develop the disease 10–30 years after the initial infection, which mainly manifests as asymptomatic aortitis, aortic valve insufficiency, coronary artery stenosis, aortic aneurysm, and mucinous myocarditis.
4. Gumma, also known as gummy tumor, is more common in the late stages of syphilis and is highly destructive. In the early stage, it is a deep, subcutaneous nodule that gradually grows and adheres to the skin. The central site gradually softens, ulcerates, and releases viscous, gum-like pus; hence, it is named gumma. It can also occur in organs like liver, bone, eyes or testis.
5. Congenital Syphillis – transmission of the disease from syphilitic mother to the fetus through the placenta. The following may result:
a. Some of the fetus may die, others are still born alive.
b. Others may be born alive with symptoms like Interstitial keratitis, Hutchinson’s teeth, Saddle nose, Periostitis, CNS anomaly.
TREPONEMA CARATEUM
1. The word “pinta” is taken from the Spanish verb “to paint” and is indicative of the various colors seen as the skin lesions mature like red, white, violet, blue, brown, or black.
2. Pinta is transmitted through contact with broken skin, and the primary lesion occurs mainly on the lower leg, dorsum of the foot, forearm, or back of the hands.
a. One to 8 weeks after inoculation, a tiny erythematous papule or cluster of papules appears and then enlarges and coalesces. An irregular and heaped border surrounds the erythematous, scaly central lesion.
b. Dissemination from the primary site results in secondary skin lesions known as pintids, which develop 3 to 9 months after the initial inoculation and before the primary lesion has healed completely. Secondary lesions are indistinguishable clinically and histologically from the primary lesion.
TREPONEMA DENTICOLA
Characteristics:
1. It can colonize new sites, penetrate deep periodontal pockets, and penetrate epithelial layers.
2. It can interact synergistically with other periodontal pathogens on several levels.
3. It could form biofilms and a range of cell–surface proteins to dysregulate the host defense to help protect the subgingival biofilm and cause host tissue destruction.
4. Together with Porphyromonas gingivalis & Tannerella forsythia, they constitute the “red complex,” a prototype polybacterial pathogenic consortium in periodontitis. One of the unifying features of the Red Complex bacteria that are responsible for chronic periodontitis progression is their high levels of extracellular proteolytic activity that is mediated by cell-surface-located proteases.
5. The treponemal outer sheath does not have a typical LPS, and the treponemes lack genes encoding the necessary enzymes for LPS synthesis. The Treponema denticola LOS has a diacylglycerol lipid anchor plus a core region consisting of hexose–hexosamine–hexose, but lacks heptose, 3–deoxy–D–manno–2–octulosonic acid, and β–hydroxy fatty acids, which are core components of LPS. Strikingly, the presence of a glycerol–hexose unit and two glycerol-hexadecanoic acid fragments in the lipid anchor indicates a glycolipid membrane anchor typically found in the lipoteichoic acid of Gram-positive bacteria. Treponema denticola LOS also stimulates fibroblasts, inducing them to produce a variety of inflammatory mediators, interleukin–6 (IL–6), IL–8, monocyte chemoattractant 1, nitric oxide, and prostaglandin E2, as well as matrix metalloproteinase 3 (MMP–3).
6. It has been shown to adhere to fibroblasts and epithelial cells, as well as to extracellular matrix components present in periodontal tissues, and to produce several deleterious factors that may contribute to the virulence of the bacteria. These bacterial components include outer–sheath–associated peptidases, chymotrypsin–like and trypsin–like proteinases, hemolytic and hemagglutinating activities, adhesins that bind to matrix proteins and cells, and an outer–sheath protein with pore–forming properties.
7. Treponema denticola is the only known oral bacterium to contain the three-step pathway required to produce H2S, from the abundant host tripeptide, glutathione. This pathway contains cysteinylglycinase, γ–glutamyltransferase, and the novel enzyme, cystalysin. H2S production via cystalysin has been shown to be the mechanism by which Treponema denticola disrupts erythrocyte membranes, thereby explaining its original description as a hemolysin.
Virulence Factors of Treponema denticola:
1. Dentilisin – is an active cell–surface–located protease that cleaves at phenylalanyl/alanyl and prolyl/alanyl bonds. It contributes to disease progression by disrupting or modulating intercellular host signaling pathways and degrading host cell matrix proteins. Dentilisin potentially allows for penetration of epithelial cell layers by Treponema denticola by degradation of intercellular adhesion proteins and modulates host cell immune responses by degradation of interleukin-1β (IL-1β), IL-6, tumor necrosis factor alpha (TNF-α), and monocyte chemoattractant protein. Dentilisin has also been reported to function in the hydrolysis of collagen.
2. Msp (major surface protein) – a member of the Tpr (Treponema pallidum repeat) protein family, is the most abundant protein in the Treponema denticola outer membrane (or sheath). Msp has been proposed to mediate colonization of host tissues and has cytopathic pore–forming activity against cultured epithelial cells. Msp is one of the immunodominant Treponema denticola antigens recognized by human serum antibodies.
3. Opp A – can bind soluble host proteins such as plasminogen and fibrinogen, but not immobilized insoluble host proteins or epithelial cells. It has been proposed to act as an adhesin and to help decorate the surface of T. denticola with host proteins as a means of avoiding or delaying immune recognition.
4. Factor h–binding protein B (FhbB) – likely to be linked to epithelial cell binding and invasion, subversion of the complement cascade, or tissue invasion.
5. Outer membrane vesicles (OMVs) – considered potent virulence factors, since they possess adhesins, toxins, and proteolytic enzymes, can mediate bacterial aggregation and invasion, are cytotoxic, and can modulate the host immune response. OMVs also facilitate the remote delivery of labile signaling molecules and prevent their degradation by other microorganisms.
BORRELIA
Characteristics:
1. The cells are helical with regular or irregular coils, 0.2-0.3 µm in diameter and 10-40 µm in length. Cells do not have hooked ends. They have an inner and outer membrane with periplasmic flagella with 7 to 20 subterminal insertion points.
2. They have linear chromosomes and plasmids with hairpin telomeres.
3. The diamino acid of the peptidoglycan is ornithine and lacks lipopolysaccharide.
4. They are microaerophilic and motile.
5. They can be visualized through aniline dyes.
6. Most members of the family cultivable in complex media that includes N-acetylglucosamine. Optimum growth is between 33 and 38°C.
7. Relapsing Fever (RF) borrelia are motile, chemo-organotrophic, microaerophilic and host-associated bacteria. The spiral body tends to be shorter than in the Lyme group Borreliae, and it lacks cytoplasmic tubules. Several endoflagella (15–20) wind around the protoplasmic cylinder and overlap in the middle. Sections of cells reveal a triple-layered outer membrane.
8. Members of the family are host–associated organisms that are transmitted between vertebrate reservoirs by a hematophagous arthropod, in all but one case, a tick.
9. Members include the agents of relapsing fever, Lyme disease, and avian spirochetosis.
10. In contrast to Treponema pallidum, Borrelia has a unique nucleus containing a linear chromosome and linear plasmids.
11. Jarisch–Herxheimer reaction is observed in patients after initiation of antibiotic therapy.
|
THREE
MAIN GROUPS OF BORRELIAE |
||||
|
Groups |
Subgroups |
Humans |
Clinical
Aspect |
|
|
EM |
Fever |
|||
|
Lyme Group |
Organotropism |
Yes |
Yes |
No |
|
High Spirochaetemia |
Yes |
Yes |
Yes |
|
|
Baggio–Yoshinari |
Yes |
Yes |
Yes |
|
|
Relapsing Fever (RF) Group |
STBRF |
Yes |
No |
Yes |
|
HTBRF |
Yes |
No |
Yes |
|
|
LBRF |
Yes |
No |
Yes |
|
|
Avian RFG |
Unknown |
|||
|
Echidna–Reptile Group |
|
Unknown |
||
Classification of Relapsing Fever (RF) Group according to vector transmission:
1. Louse–borne relapsing fever (LBRF) Group
Louse–borne Relapsing Fever (LBRF) is an epidemic disease linked to war, famine, refugees, poverty, and poor sanitation.
The epidemic form is caused by Borrelia recurrentis, for which the vector is the human body louse (Pediculus humanus humanus or Pediculus humanus corporis). It occurs from human to human through lice, which ingest infected blood and transmit the spirochaetes to a new host through the skin or mucous membranes when the body of the louse itself is crushed by scratching.
Epidemic Relapsing fever is characterized by a short, febrile paroxysm lasting 2 or 3 days, alternating with afebrile periods of 3 or 4 days and resulting in 2 to 10 relapses, more commonly the lesser number, each attack terminates by crisis.
2. Soft–tick–borne relapsing fever (STBRF) Group
Vectors of the STBRF are argasid ticks of the genus Ornithodorus species which lack the dorsal shield. STBRF spirochetes adapt and colonize the salivary glands of Ornithodoros specie in the long term and are maintained trans-stadially and transovarially. The saliva of Ornithodoros species supports the feeding process by providing a cocktail of anti-hemostatic, anti-inflammatory, and immunomodulatory molecules.
The infectious cycle of argasid–transmitted RF spirochetes requires adaptation to three environments, namely the midgut and salivary glands of the tick and the vertebrate host.
a. Old World Strains – Borrelia crocidurae, Borrelia duttonii, and Borrelia hispanica
b. New World Strains – Borrelia hermsii, Borrelia parkeri, and Borrelia turicatae
Endemic Relapsing Fever is characterized by long, febrile paroxysm lasting 2 to 7 days of illness, alternating with afebrile periods of 4 to 14 days.
3. Hard–tick–borne relapsing fever (HTBRF) Group
HTBRF Borreliae are transmitted by several genera of hard ticks, notably Ixodes species, Amblyomma species, Dermacentor species, and Rhipicephalus species.
Borrelia miyamotoi is a spirochaete of the RF group, transmitted by the same hard ticks (Ixodes sp.) of the Borreliae Lyme group.
The clinical manifestations in humans are characterized by fever, chills, nausea, headache, myalgia, skin rash, and lymphadenopathy. In immunocompromised patients, meningoencephalitis can also be observed. Unlike STBRF, a small number of patients experienced more febrile episodes.
Glycerophosphodiester phosphodiesterase (GlpQ) is an enzyme that is absent in the Borrelia Lyme group and used in the differential diagnosis. GlpQ is also found in other relapsing fever Borrelia species. GlpQ is also produced by Mycoplasma pneumoniae.
4. Avian Relapsing Fever Group
Borrelia that infects birds. Borrelia anserina is the infectious agent of the avian spirochetosis.
BORRELIA BURGDORFERI
1. Transmitted to man by Ixodes dammimi and Ixodes pacificus that causes the Lyme disease, however, the Baggio–Yoshinari Syndrome (BYS), a disease that mimics the Lyme disease is transmitted by hard Ixodid ticks of the genera Amblyomma, Rhipicephalus and Dermacentor.
2. A plasmid–encoded nicotinamidase (PncA) enzyme is essential for infectivity of Borrelia burgdorferi in a mammalian host. It is also involved in the production of NAD.
3. It causes a disease (Lyme Disease) with three stages:
a. In the first stage, shortly after and in the area of a tick bite, a non-pruritic rash (erythema migrans) appears and spontaneously disappears after a few weeks.
b. The second stage is frequently associated with neurological complications such as lymphocytic meningitis and focal and multifocal peripheral and cranial neuropathies; characteristic manifestations are unilateral or bilateral facial palsy and radiculitis.
Bannwarth syndrome (BWS) is a term applied to the constellation of painful radiculoneuritis characterized as severe, burning, often dermatomal pain. In most cases, BWS affects the limbs, with only a few reported cases of sacral radiculitis causing neurogenic urinary dysfunction.
c. The third stage is associated with severe neurological complications, including encephalopathy, encephalomyelitis, and predominantly sensory axonal polyneuropathy. A lymphocytic pleocytosis in CSF and demonstration of Borrelia burgdorferi infection in serum or CSF are the main laboratory findings.
d. Other species that cause LD are Borrelia afzelii, Borrelia garinii, Borrelia valaisiana, Borrelia spielmanii, Borrelia bissettii, Borrelia lusitaniae. Borrelia mayonii is another species which is capable of producing Lyme Disease but unlike B. burgdorferi, however, B. mayonii is associated with nausea and vomiting, diffuse rashes (rather than a single so-called “bull’s-eye” rash), and a higher concentration of bacteria in the blood.
4. The Baggio–Yoshinari Syndrome (BYS) is an infectious disease that mimics the Lyme Disease (LD). It is distinguished from LD by the following aspect:
a. It is transmitted by ticks not belonging to the genus Ixodes.
b. The etiological agent is not isolated or cultured in BSK II-modified medium, and currently, only identified by PCR procedures.
c. Spirochete, presenting typical, corkscrew morphology with spiraled movement found in LD patients, was never determined in BYS patients. Researchers suggest that spirochetes in BYS exist in atypical round-shaped forms or bacteria-like morphologies.
d. Borrelia burgdorferi in BYS patients gives rise to low immune humoral and cellular responses. Antibody titers are low and disappear fast in the serum of patients.
e. BYS patients present all the clinical aspects displayed by LD; however, some divergences are noted, such as the high frequency of clinical recurrences, the necessity of prolonged antibiotic therapy administered at disseminated disease stages and high risk of emergence of autoimmune and chronic fatigue symptoms.
5. The BYS presents two main stages:
a. The initial phase, or infectious stage, starts after the tick bite and inoculation of Borrelia burgdorferi in the skin (localized stage), which is followed by dissemination. During this stage, the spirochetes move to the different organs through the vascular or lymphatic circulation systems. On most occasions, the infection improves spontaneously.
b. The secondary stage occurs when the microorganisms cause inflammatory processes and damage to many organs or tissues such as the joints, the heart, the peripheral and central nervous system, the eyes, and the skin.
c. Eventually, spirochetes may remain dormant, and the infection can linger in a latent stage for months or even years. However, at any moment, it can re-activate, causing the disease to progress into the tertiary stage of infection.
d. One interesting aspect observed in BYS patients is the high incidence of ocular involvement. In addition to disorders related to abnormalities of the ocular, causing diplopia, anisocoria, eyelid ptosis, squinting, mydriasis and ophthalmoplegia, intrinsic ocular lesions such as uveitis, retinal arteritis, and papilledema were also identified.
e. A very common and peculiar finding observed in BYS is the appearance of relapsing skin lesions, resembling EM, or multiple and disseminated maculo-erythematous lesions, which could be confused with the symptoms of the early stage of Borrelia burgdorferi infection. These reactive skin lesions are not generally followed by flu-like symptoms or systemic manifestations. In most cases, they appear when patients are debilitated, or can be triggered by physical stress such as exposure to high temperatures, for example, after having a hot bath. These types of skin lesions have not been reported in LD patients so far; therefore, it was described as reactive exanthema.
Laboratory Tests:
1. Histochemical procedures using:
a. Aniline Dyes (Gram, Wright, Wright–Giemsa, Giemsa, and polychromes)
b. Fluorochromes (Thioflavin–T, Acridine orange, and Rhodamine)
c. Silver impregnation techniques (Warthin–Starry, modified Dieterle, modified microwave Dieterle, and Bosma–Steiner)
d. Immunocytochemical methods (Polyclonal and monoclonal antibodies)
Giemsa–stained thick blood smear. Borreliae are best detected in blood obtained while a patient is febrile. During subsequent febrile episodes, the number of circulating spirochaete decreases, making it harder to detect them on peripheral blood smear.
2. Standard two–tiered testing (STTT) is the recommended algorithm for laboratory diagnosis of Lyme disease (LD). Several limitations are associated with STTT that include low sensitivity in the early stages of disease but >99% sensitivity for detecting late infection. Another limitation is the technical complexity and subjectivity associated with second–tier immunoblotting.
a. The first–tier Enzyme Immunoassay (EIA) quantifies potential antibodies against Borrelia burgdorferi. If the EIA is positive or equivocal,
b. Second–tier immunoblotting is performed to detect antibodies against more specific Borrelia burgdorferi surface proteins.
Both tiers must be considered positive for laboratory support of an LD infection, and the second tier is positive if either an IgM and/or IgG immunoblotting is positive, with IgM immunoblotting testing evaluated only on samples from patients with a duration of illness of ≤30 days.
3. Modified two–tiered testing (MTTT)
a. The first MTTT algorithm uses a whole cell sonicate (WCS) EIA as the first test that, if positive or equivocal, is followed by the C6 EIA.
b. The second MTTT uses a whole-protein VlsE (variable major protein-like sequence, expressed) CLIA (chemiluminescence immunoassay) that, if positive or equivocal, is followed by the C6 EIA.
For a patient to be considered positive for LD when tested by either of the MTTT algorithms, both tests need to be equivocal or positive. MTTT cannot distinguish active and past infections and cannot diagnose reinfection because antibody responses can persist for years.
The three markers that have high sensitivity for the detection of anti – Borrelia burgdorferi antibody in serum from patient with early LD are VlsE, OspC-K, PepVF.
4. Identification of Glycerophosphodiester phosphodiesterase (GlpQ) enzyme
5. Culture using:
a.
Barbour–Stoenner–Kelly
(BSK) media
b. Noguchi medium (with ascitic
fluid)
c. Kelly–Pettenkofer
modified medium (MKP)
LEPTOSPIRA
Characteristics:
1. They are tightly coiled spirochetes with very fine spirals. One end of the organism is often bent, forming a hook.
2. They appear as minute cocci in chain as seen in the Darkfield Microscope.
3. They are strictly aerobic, oxidase (+), catalase (+) and peroxidase (+).
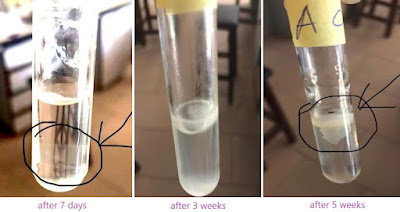
4. They grow best in protein rich semisolid medium (Fletcher’s) where they produce round colonies. Their growth reaches a maximum density in a discrete zone beneath the surface of the medium, which becomes increasingly turbid as incubation proceeds. This growth is related to the optimum oxygen tension and is known as a Dinger's ring or disk.
5. They can survive for weeks in water with slightly alkaline pH.
6. They are divided into two species with different metabolic properties:
a. Leptospira
interrogans which include the pathogenic strains.
b. Leptospira biflexa which includes saprophytic strains.
Leptospira biflexa was differentiated from Leptospira interrogans by the growth of the former at 13°C and growth in the presence of 8-azaguanine (225 μg/ml) and by the failure of Leptospira biflexa to form spherical cells in 1 M NaCl
LEPTOSPIRA INTERROGANS
This organism is found in proximal tubules of kidneys of infected animals and is passed on to humans through abrasions of skin or mucous membranes. So, human infection results from contact with animal urine or water which has been contaminated with urine like soil, natural water (flood), foodstuff. Leptospirosis develops after an incubation period of 10–12 days.
The signs and symptoms vary from a mild fever to severe illnesses including jaundice, kidney failure and meningitis.
|
L.
interrogans serogroup |
Human
Disease |
Clinical
Findings |
|
icterohemorrhagiae |
Weil’s disease |
jaundice, hemorrhages, aseptic meningitis |
|
autumnalis |
Fort Bragg Fever |
fever, rash over tibia |
|
canicola |
Infectious jaundice |
influenza–like illness, aseptic meningitis |
|
grippotyphosa |
Marsh fever |
fever, prostration, aseptic meningitis |
|
hebdomadis |
Seven day fever |
fever, jaundice |
|
pomona |
Swineherd’s disease |
aseptic meningitis |
Two types of Leptospirosis:
1. Anicteric leptospirosis – a mild, self–limiting form of leptospirosis. It is characterized by fever, conjunctival suffusion, severe myalgia, skin rash, lymphadenopathy, hepatomegaly, splenomegaly, and meningitis. It is composed of two phases:
a. Acute Phase or Leptospiremic Phase or Septicemic Phase – usually starts between 2 to 14 days after Leptospira infection and lasts between 3 to 10 days. In this phase, bacteria in the bloodstream are moving to different organs.
b. Immunologic Phase – in this phase, the bacteria has moved from the blood to the organs. The bacteria are most concentrated in the kidneys.
2. Icteric leptospirosis (Weil’s Disease) – severe form of leptospirosis characterized by renal failure, hepatic dysfunction, thrombocytopenia, and hemorrhagic complications. There is presence of jaundice, persistence of fever, azotemia, uveitis, hemorrhage, vascular collapse.
Laboratory Tests:
1. The reference method for serological diagnosis of leptospirosis is the Microscopic Agglutination Test (MAT), in which patient sera are reacted with live antigen suspensions of leptospiral serovars. After incubation, the serum–antigen mixtures are examined microscopically for agglutination, and the titers are determined. Formerly, the method was known as the agglutination–lysis test because of the formation of lysis balls or lysis globules of cellular debris in the presence of high–tittered antiserum. However, these are tightly agglutinated clumps of leptospires containing live cells and not debris. MAT serology is insensitive, particularly in early acute-phase specimens. Moreover, patients with fulminant leptospirosis may die before seroconversion occurs.
Other Serologic Test includes IgM Leptocheck, IgM ELISA,
2. Darkfield microscopy – fluorescent antibody, silver impregnation/ staining with aniline dye.
3. Culture
a. Ellinghausen–McCullough–Johnson–Harris (EMJH) medium – a semisolid medium containing oleic acid and albumin with STAFF (sulfamethoxazole, trimethoprim, amphotericin B, Fosfomycin and 5–fluorouracil) added to prevent growth of other bacteria.
b. Tween 80 albumin, Stewart’s medium, Korthof medium, Fletcher’s – contains rabbit serum as the added enrichment.


No comments:
Post a Comment