The majority of leukocytes
are formed from primitive mesenchymal cells in the hematopoietic tissues. As
the cells mature from their fixed or relatively fixed “blast” and “pro” stages
to mature and morphologically identifiable types, they lose their intercellular
connections, and acquire amoeboid activity. These cells after reaching the more
mature stage, escape from the tissue by means of their own mobility into the
circulating blood.
Leukocytes are lighter
than red cells and tend to accumulate at the periphery of the flowing blood
adjacent to the lining of the blood vessel where they tumble along at a slower
rate than the axial period of the blood column. Some of the leukocytes are
continually squeezing between the endothelial cells and the walls of the capillaries
into the tissue spaces. From the tissue spaces, they may pass into the
lymphatic channels and thus get back into the blood stream. At any given time,
there are numerous leukocytes that have escaped from the hematopoietic organs
and are not in circulation. These cells are readily available on demand are
called back into the active circulation when there are chemotactic substances
in the lumen of the vessels which attract the leukocytes in the perivascular
areas.
Leukocytes after delivery
into the blood stream and after surviving for a number of days in the body,
eventually become senile and die. These effete cells are phagocytized by other
cells in the blood stream by the phagocytic cells of the tissue spaces, by
macrophages of the splenic pulp or by the littoral cells of the liver sinuses.
Leukocytes in addition to
being destroyed in the body, are continually escaping from the body by passing
into secretions of various glands or by passing between the cells lining the
respiratory, gastrointestinal and genitourinary tracts into the lumen of these
organs. Thus, we find leukocytes in all body fluids including sweat, synovia,
pancreatic juices, feces, urine and secretions from the genital tracts. In
inflammatory, ulcerative and hemorrhagic lesions involving any of the excretory
organs there is an increased rate of loss of leukocytes from the body.
MATERIALS NEEDED FOR
FORMATION OF WHITE BLOOD CELLS
In general, the leukocytes
need essentially the same vitamin and amino acids as most of the other cells of
the body for their formation. Especially does lack of folic acid, a compound of
the Vitamin B complex, block the formation of white blood cells as well as
prevent maturation of red cells.
CHEMISTRY OF
LEUKOCYTES
1. Granulocytes
Granulocytes
process glucose by aerobic glycolysis to yield lactic acid. Alkaline
phosphatase is present in increased concentration in granulocytes during
infections and decreased in granulocytic leukemia. Acid phosphatase is
increased in chronic granulocytic leukemia and normal in infestations.
Phospholipids, lysozyme and phagocytin are bactericidal and may also be found
in granulocytes. In addition, peroxidase, lipase, sulfhydryl groups, heparin,
histaminase, glucogen, dipeptatases, tripeptases, maltose, beta glucuronidase
and glucuronic acid are also present in granulocytes.
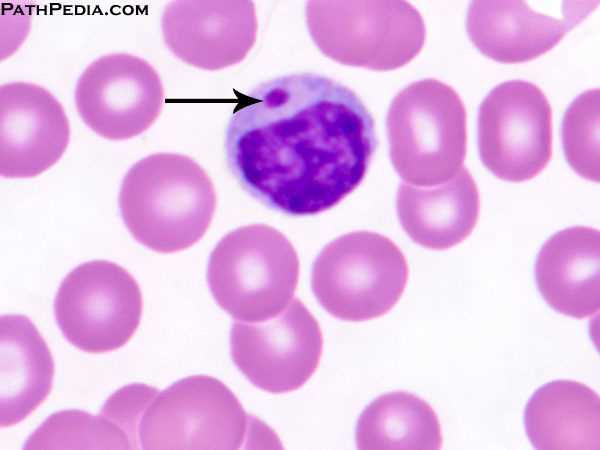
2. Lymphocytes
Glycogen
and acid phosphatase are found in lymphocytes. They may also contain alkaline
phosphatase, dipeptidase, oxidase and peroxidase.
3. Monocytes
Glycogen,
sudanophilic substances, lysozyme, acid phosphatase, phospholipids and lipids
are present in monocytes.
4. Plasma cells
Plasma
cells contain large amount of RNA and DNA and are responsible for the
manufacture of antibodies.
LIFE SPAN OF
LEUKOCYTES
The main reason leukocytes
are present in the blood is simply to be transported from the bone marrow or
lymphoid tissue to the areas of the body where they are needed. Therefore, it
is to be expected that the life of leukocytes in the blood would be short.
Granulocytes –
2 – 3 hours during serious tissue
infection
–
14 hours (average) usually
–
several days, when not needed in
the tissues.
Monocytes –
still a mystery, for the wander
back and forth between
the tissues
and the blood
Lymphocytes –
in the blood, only a few hours
–
using radioactive lymphocytes –
100 to 200 days
depending
on the tissues need for the cells.
PROPERTIES OF
LEUKOCYTES
1. Diapedesis –
the leukocytes can squeeze through the pores of the blood vessels by the
process of diapedesis. That is, even though a pore is much smaller than the
size of the cells, a small portion of the cell slides through the pore at a
time, the portion sliding through being momentarily constricted to the size of
the pore.
2. Amoeboid movement – one the cells have entered the tissue spaces, the polymorphonuclear
neutrophils, the lymphocytes and monocytes to a lesser degree, move through the
tissues by amoeboid motion.
3. Chemotaxis –
a number of different chemical substances in the tissues cause the leukocytes
to move either toward or away from the source of the chemical. This phenomenon
is known as chemotaxis. Degenerative products of inflamed tissues, bacterial
toxins can cause chemotaxis of leukocytes.
Positive
chemotaxis – when cells are attracted
toward the source of the chemical substance
Negative
chemotaxis – when the leukocytes are
repel from the source of the chemicals.
4. Phagocytosis
– ingestion of particulate matter by the cells. Whether or not phagocytosis
will occur, depends upon three selective procedures:
a. If the surface of the particle is
rough, like hood of phagocytosis is increased, whereas a smooth particle is
resistant to phagocytosis.
b. Most natural substances of the
body have electronegative surface charge, therefore are repelled from the
phagocytes, which also carry electronegative surface charges. Dead tissues and
foreign particles are frequently electropositive and are therefore subject to
phagocytosis.
c. The body has a means for
promoting phagocytosis of foreign materials by selectively combining foreign
particles with globulin molecules called opsonins.
TOTAL LEUKOCYTE
COUNT
Adults 5,000 – 10,000 / cu.mm 5 – 10 x 109/L
Infants 6,000 – 18,000/ cu.mm 6 – 19 x 109/L
Children 5,000 – 15,000/ cu.mm 5 – 15 x 109/L
FUNCTIONS OF
NEUTROPHILS
1. Prevent or retard the intrusion of infectious agents and other foreign
materials into the host environment. This is accomplished by phagocytosis and
digestion of the material.
2. Secretory function – neutrophils release an enzyme known as lysozyme
which acts as a hydrolyzing agent and is important in the destruction of
certain bacteria.
3. They also liberate immune bodies and other enzymes that interferes
bacterial growth.
4. Neutrophils exhibit amoeboid motion and play a role in inflammatory
process. They release endogenous pyrogen that produces fever by acting on the
hypothalamus to set the body’s thermostat at a higher level.
FUNCTIONS OF
EOSINOPHILS
1. Interact with foreign protein (they detoxify protein) under the control
of adrenal cortical hormone.
2. They exhibit chemotaxis. They are attracted to fibrin or proteolytic
enzyme. Among the chemotactic factors that attract eosinophils is present in
basophils and mast cells.
3. Eosinophils phagocytose foreign particles and antigen – antibody
complexes.
4. Eosinophils contain substances that inactivate factors released by mast
cells and basophils, such as histamine, slow reacting substances of
anaphylaxis, and platelet – activating factor.
5. They produce antihistamine and are associated with allergy.
6. They provide some defense against helminthic parasites.
7. Eosinophils are sources of plasminogen
FUNCTIONS OF
BASOPHILS
1. Basophils respond to adrenal cortex hormones in similar fashion to
eosinophils.
2. They liberate heparin, histamine, hyaluronic acid and serotonin.
3. Basophils synthesize and store histamine and eosinophil chemotactic
factor anaphylaxis.
4. They appear to be involved in immediate hypersensitivity reactions,
such as allergic asthma.
5. Speculations suggest that basophils are associated with fibrinolysis.
6. Lipid metabolism and anaphylactoid reactions
7. Secretory functions – basophils release their granule contents outside
the cells, after exposure to stimuli.
Note:
Acid mucopolysaccharide is responsible
for the metachromatic staining property
of Basophil granules
FUNCTIONS OF
MONOCYTES
1. Monocytes are formed in the marrow, transported by the blood, and
migrate into the tissues where they transform into histiocytes or macrophages,
to spend the majority of their life span. The blood monocytes and tissue
macrophages make up a mononuclear phagocyte system (reticuloendothelial
system). This system has an important role in defense against microorganisms,
including bacteria, fungi, viruses and Protista.
2. The cells are motile and respond to chemotactic factors.
3. They engage in phagocytosis, a process that is enhanced if the particle
is coated by IgG or complement for which the macrophages have membrane
receptors. These mononuclear phagocytes are an integral part of both humoral
and cell – mediated immunity.
4. Play a role in the synthesis and secretion of transferrin, interferon,
endogenous pyrogen, lysozyme.
5. Macrophages remove and process senescent cells and debris through
phagocytosis and digestion.
6. They act as feeder cells (trephocytes) supplying iron to red cells and
protein to antigenic sites to plasmacytes and lymphocytes.
7.
They play an important role in the regulation of hematopoietic
activity.
FUNCTIONS OF LYMPHOCYTES
1. The lymphocyte has a primary function in cell–mediated immunity, which
includes delayed hypersensitivity; graft rejection, graft versus host
reactions, defense against intracellular organisms such as tubercle bacilli and
Brucella and probably defense against neoplasms.
2. B cells and their pyrogeny perform in humoral immunity, or in the
production of antibodies, either as a lymphocyte or after transformation into
plasmacyte.
3. They act as feeder cells (trephocytes) – play a role in the synthesis of
protein, enzymes, minerals and transport them to the sites of cellular growth.
4. Play a role in chronic inflammatory process.
T
cells – lymphocytes influenced by the thymus (thymus dependent)
B
cells – lymphocytes influenced by the bursal equivalent organ (bursa dependent)
FUNCTIONS OF
PLASMACYTES
1. Plasmacytes play a role in antibody formation. They produce
immunoglobulin for secretion outside of the cell.
The
so called antigen–antibody quartet:
a. Lymphocytes
b. Monocytes
c. Eosinophils
d. Plasma cells
MORPHOLOGIC
ABNORMALITIES OF LEUKOCYTES
Hereditary conditions
affecting leukocytes:
1. Pelger–Huet anomaly – also called “hereditary hyposegmentation” hereditary autosomal
dominant condition characterized by hypolobulation of the granulocyte or
failure of normal segmentation of granulocytic nuclei. Most nuclei are
band–shaped, rod –like dumbells or peanut–shaped, “spectacle–like” or
“pince-nez” nuclei with smooth, round or oval individual lobes and pyknotic
nuclear chromatin.
2. Alder’s anomaly or Alder–Reilly anomaly – recessive trait characterized by the presence of
larger than normal azurophilic and basophilic granules confused with toxic
granulation but is unrelated to infection and is not transient. Cells usually
affected are PMN, lymphocyte and monocyte.
3. May–Hegglin anomaly – rare autosomal dominant condition characterized by the presence of
pale blue inclusions resembling Dohle bodies in neutrophils, giant platelets
and in some persons, thrombocytopenia. The inclusions are larger and more
prominent than the Dohle bodies found in infections. Cells usually infected are
eosinophils, basophils, monocytes and neutrophils.
4. Chediak–Higashi anomaly – also known as Chediak–Steinbrick Anomaly
–
congenital gigantism of peroxidase granules.
–
autosomal recessive disorder characterized by partial albinism,
photophobia, Increased
susceptibility to infection and presence
of very large granules which appear
to be abnormal lysosomes.
–
cells affected are granulocytes, monocytes and lymphocytes
5.
Jordan’s anomaly – characterized by vacuolization of leukocytes
–
vacuoles are present in the cytoplasm of granulocytes, monocytes and
occasionally
lymphocytes and plasma cells of patients with progressive muscular dystrophy.
6. Hereditary neutrophilic hypersegmentation – hyperlobulation of the nuclei of the granulocytes
from 4 – 6 lobes or more with no evidence of Vitamin B12 and / or
folic acid deficiency
7. Hereditary giant neutrophilic leukocytosis – rare hereditary disorder where there is a tendency
to produce polyploid cells. Characterized by presence of neutrophils and
hyperlobulation of nuclei.
ABNORMAL INCLUSION
BODIES FOUND IN LEUKOCYTES
1. Auer bodies or Auer rods –
with Romanowsky stains, Auer rods are linear or spindle–shaped red–purple
inclusions in myeloblast and monoblast. Auer rods are derivatives of
azurophilic granules and stain positively for Sudan Black B, myeloperoxidase,
chloroacetate, esterase and acid phosphatase. They are caused by unusual
development of lysozymes.
2. Toxic granules – toxic
granules are dark blue to purple cytoplasmic granules in the metamyelocyte,
band or neutrophilic stage. These are characteristics of bacterial infections
and are frequently seen in aplastic anemia and also in myelosclerosis.
3. Dohle bodies – these are
small round or oval bodies up to 2 – 3 micrometers in size, usually in the periphery
of the cytoplasm of neutrophils, which stain blue–gray with Romanowsky dye.
These are mostly seen in bacterial infections, severe burns, exposure to
cytotoxic agents and uncomplicated pregnancy. They are remnants of free
ribosomes or rough surfaced endoplasmic reticulum persistent from an earlier
stage of development.
4. Snapper–Schneid bodies –
inclusion bodies found in the cytoplasm of multiple myeloma and plasma cells
after therapy with amidine drugs.
5. Russell or Fuch’s bodies –
gamma globulin bodies in the cytoplasm of plasma cells and inflamed tissue. The
bodies give the cells a grape or berry or morula cell appearance.
OTHER ABNORMALITIES
IN THE NUCLEUS AND CYTOPLASM OF LEUKOCYTES
1. Hypersegmented neutrophil –
also called P.A. polycell of macropolycyte; larger than normal neutrophil and
has 5 – 10 segments; seen in pernicious anemia
2. Polycyte – has a normal size
but with 4 – 6 lobes in the nucleus; found in stage of recovery from infection.
3. Pyknotic cell – cell whose
nucleus becomes smaller and denser, nuclear segments disappear, leaving several
balls of dense chromatin.
4. Virocyte or atypical lymphocyte or Downey type cell or Turk irritation
cell – cell has a chromatin
arrangement which gives the cell a “moth–eaten” or “tunneled” appearance or
“Swiss–cheese” form; vacuolated which gives the cell a “foamy” or “bubbly”
appearance; cell has prominent axurophilic granules
Downey
type I – cell with deeply indented
nuclei
Downey
type II – cell with smooth cytoplasm
with patchy peripheral and radial basophilia has been called “stress”
lymphocyte; seen in infectious mononucleosis, viral pneumonia, herpes zoster,
herpes simplex and other viral infections
5. Rieder cell – myeloblast that
is characterized by having a nucleus with deep indentations often suggesting
lobulations; seen in acute myeloid leukemia.
6. Vacuolated cell – cell with
holes or vacuoles in the cytoplasm; vacuoles are signs of degeneration in
severe infection, chemical poisoning, leukemia; if seen in normal blood,
indicative of smear prepared from over two – hour old oxalated blood.
7. Cells exhibiting phagocytosis
– cells that are endowed with the ability to engulf particles are called
phagocytes. In general, these include the polymorphonuclear granulocytes
(neutrophils and eosinophils), the monocytes in the formation of Lupus
erythematosus (L.E.) cells and Tart cells.
8. Basket cell – net like
nucleus from a ruptured white cell; in normal blood it is believed to be the
older form of smudge cell.
IRREGULARITIES IN
THE BLOOD SMEAR PREPARATION AFFECTING LEUKOCYTES
1. Squashed or distorted lymphocytes – caused by excessive pressure on the cell during the
process of preparation.
2. Accumulated white cell – a bunch of white cells seen on the edge of a blood
smear and caused by improper spreading technique during smear preparation.
3. Smudge cell
– a bare nucleus of a ruptured white cell caused by excessive pressure on the
cells during smear preparation. This is indicative of increased fragility of
cells or abnormal destruction of cell.
4. Disintegrated or ruptured cell – this is caused by excessive pressure on the cells
during smear preparation and is found on the smear prepared from old blood. It
is also found in toxic conditions.
5. Poorly stained leukocytes – this maybe caused by:
a. Incorrect pH of buffer
b. Improper mixing of stain and
buffer
c. Too short staining period.
6. Precipitated stain – this is caused by the failure to flush properly the excess stain on
the side.














No comments:
Post a Comment